caste-health-india
The Impact of Caste on Health Outcomes in India
Caste and Health in India
TABLE OF CONTENTS
BACKGROUND:
As the second-most populous nation in the world, India has made significant strides in both economic growth and health care since its establishment in 1947. Poverty rates have decreased due to anti-poverty interventions, and the average life expectancy is currently at approximately 69 years (1). While India is home to some of the best medical centers, such as the Fortis Hospital in Bangalore which has been included in global hospital rankings (2), these institutions are not a complete representation of the Indian healthcare system. A closer look at health indicators reveals a sharp divide in quality indicators along social boundaries. Low-income Indians often receive poor quality healthcare and lack access to more advanced services (3). While cities experience increased economic growth, resulting in improved healthcare services, rural areas lack health care workers and necessary infrastructure (4). Key social determinants result in the heterogeneity of health outcomes of India, with various stakeholders at play.
However, among the health inequities in India, none is so historically-ingrained and replicated as caste. While the caste-system was abolished and caste-based discrimination criminalized, it continues to impact health with regards to social mobility and opportunities (5). Even today, women in an “untouchable” caste have a lower life expectancy and reduced healthcare access compared to their upper-caste counterparts (6,7). While both caste and race are socially ascribed dimensions used to stratify individuals, caste, unlike race, is generationally inherited (8). In this project, I sought to determine whether caste was a significant predictor of three health outcomes: TB, anemia, and health-insured status, when controlling for age and wealth index and accounting for spatial factors.
Definition of Caste
B. R. Ambedkar, an Indian politician who combatted caste-based discrimination, invokes several definitions of caste in an essay titled Castes in India (9). In addition to acknowledging caste as a closed social unit, he identifies endogamy as the key trait in defining caste. Caste, unlike race, is specific to a respective society and viewed as a whole unit (i.e. an individual cannot be “half” of a caste) (10). However, both caste and race have been associated with health disparities (11,12). For the purposes of this paper, the three-tiered framework on how racism influences health will be applied to casteism’s effect on health as well: institutional, interpersonal, and internalized casteism (13).
Academics have used caste as a proxy for socioeconomic status rather than designating it separately (14)(15). However, this is flawed for two reasons. First, health disparities on the basis of caste are still prevalent, even when accounting for socioeconomic status, thus indicating they are not synonymous (16,17). Second, this does not account for a history of oppression and generational transfer of wealth which the caste system continues to perpetuate. Caste directly modifies socioeconomic status and therefore must be accounted for in health interventions.
Caste in India:
The caste system in India is a hierarchy that has been active for centuries. According to the ancient Hindu texts, there are four overarching caste categories: Brahmins (priests), Vaishyas (traders), Kshatriyas (soldiers), and Shudras (servants) (18). Those not classified in any of those options are considered the “Untouchables”, i.e. the outcastes or Dalits. This power imbalance introduced caste-based discrimination. Parallel to Jim Crow laws in the United States, Dalits were prohibited from entering temples, criminalized for eating beef, and forced to use separate facilities (18). In addition to institutional oppression, Dalits experienced interpersonal discrimination. While the caste system does have an origin in the Hindu faith, caste-based discrimination was also practiced among Christians and Muslims living in India (18). In his undelivered speech, Annihilation of Caste, B. R. Ambedkar argued that caste integration would not sufficiently address caste-based discrimination (18). Rather the ultimate solution was “to destroy the belief in the sanctity of the shastras” (the shastras are defined by Ambedkar as those who “teach [individuals] this religion of caste”) (18).
When India gained independence in 1947, several pieces of legislation sought to rectify caste-based oppression. The caste system was abolished via the Indian Constitution in 1950 (19). Additionally, the Constitution explicitly defined marginalized castes as “scheduled castes” (20), A reservation policy in the Indian Constitution allows opportunities (ranging from employment to education) to be allocated in percentages for specific castes deemed as “Scheduled Castes”. Additionally, the Scheduled Castes and the Scheduled Tribes (Prevention of Atrocities) Act, which passed in 1989, outlined hate crimes against Dalits in order to protect them from violence. While these policies were well-intentioned, they lacked large-scale impact; a study evaluating the caste reservation system discovered a mere five percentage point increase in employment for Dalits (21). Dalits still experience higher poverty rates, school dropout rates, and discrimination from their higher-caste counterparts (19). Caste is still a significant determinant of employment (22) and socioeconomic status (19).
Caste as a Determinant of Health
According to Link and Phelan’s theory of fundamental causes of health (1995), a fundamental cause includes social factors, which may affect access to resources, which in turn influence affect health outcomes (23). Through this framework, caste fits the definition of a fundamental cause, as it directly affects health through material and non-material access. The mechanism through with caste influences health consists of three components: genetics, early environmental exposures, and social mobility toward obtaining resources (5). With regards to genetics, marrying outside of caste was generally frowned upon (19), resulting in genetic similarities within caste. Genome analysis proved that upper-caste groups tended to have more European DNA in comparison with lower-caste groups, which have higher amounts of Asian-originated DNA (24). Furthermore, genetically transmitted diseases have different rates in accordance to caste. For example, sickle-cell disease is more prevalent among scheduled castes, compared to upper castes (25). Additionally, early environmental exposures, such as iodine intake, have been attributed toward caste, along with their outcomes (in this case, goiters) (26). With respect to social mobility, despite the reservation policy on employment and educational opportunities, lower-caste individuals still have a lower access to increased income, though this could be attributed toward social capital as well (27). This theory aligns with the evidence presented in existing literature, which reveals caste dictates a significant role in multiple health outcomes, such as maternal morbidity (28) and anemia (29) (this will be discussed more extensively).
Infant and Child Health Outcomes
Infants and children identifying as scheduled castes face adverse health outcomes. In a study conducted in 2000, along with results from the National Family Health Survey conducted in India during 2015-2016, scheduled castes had a higher incidence of low birth weight (7,30). Additionally, they experience lower vaccination rates for basic immunizations (15,31,32). The mechanism behind this trend has been attributed toward healthcare delivery, as mothers from scheduled castes have reported decreased healthcare access and experiencing discrimination when receiving services (33). Infants of scheduled castes were also breastfed for a shorter period of time and received water as an alternative, increasing the chances of waterborne diseases (34). When this was examined, many women cited issues with lactation as the primary reason in switching from breast milk to commercial weaning products (35). Children from scheduled castes are also at a higher risk of micronutrient deficiencies, such as anemia, which can result in stunting (36,37). This trend was also observed among urban children, who generally have better health outcomes (38). Furthermore, children from scheduled castes experience goiters at higher rates due to iodine deficiency (26,39). One study attributed this nutritional disparity toward a poor socioeconomic environment, which lower-caste individuals are more likely to experience (40).
Adult Health Outcomes
Caste also plays a significant role in several health outcomes in the adult stage of the life course. Members from scheduled castes are more likely to use biomass as a fuel for cooking, which results in respiratory diseases such as tuberculosis (41). Adolescent undernutrition, also a risk factor for TB, is higher among scheduled castes (42). When evaluating a government tuberculosis reduction program, researchers discovered that members from scheduled castes also face higher levels of stigma, resulting in them delaying a sputum test and worsening their prognosis (43). Caste also impacts maternal health outcomes. Women from scheduled castes experience undernutrition, resulting in a lower maternal BMI (44). Mothers from scheduled castes were also less likely to have a birth attendant, tetanus vaccines, and antenatal care in comparison to their upper caste counterparts (45). Upon a closer examination, it was revealed that lower-caste women tend to use untrained birth attendants in order to avoid caste-stigma perpetuated by medically trained birth attendants from upper castes. This could possibly be linked to higher rates of stillbirth among scheduled caste women (46). Women from lower-castes also experience higher rates of intimate partner violence (7,47), which has been linked to several health outcomes such as reproductive disorders and psychological conditions (48). Researchers have attributed caste inequalities to increased rates of IPV (49). Even after controlling for socioeconomic status, members of scheduled tribes face a lower life expectancy compared to their upper caste counterparts (50).
Institutional Barriers
Structural obstacles need to be considered when evaluating caste’s role in health. In the National Family Health Survey, approximately 70% of Scheduled Caste respondents experienced at least one major issue in accessing health care (7). Members of scheduled castes are more likely to use public health care services in comparison to upper caste individuals, which are generally of lower quality (4,51). The reason behind this could be tangential to healthcare funding in India, which mostly consists of out of pocket expenditures (4). Given that many scheduled castes live in poverty, this would inevitably result in lower-quality health services (52). This is further supported by the narratives of Dalits, who cited poverty as a reason for lack of biomedical care (53). Another obstacle cited was distance from health care facilities, in which individuals belonging to scheduled castes were located further from services (7,54). Interpersonal casteism was also prevalent: lower caste women were more likely to experience discrimination (55).
Systemic barriers are not limited to health care systems. Additional systems that influence health include water and sanitation. In a study comparing villages, Dalit communities had fewer toilets and were forced to defecate in the fields (56). As a result, they had a higher incidence of waterborne diseases due to increased microbial content in their drinking water.
METHODS:
For this project, I used the 2015-2016 cohort of the Indian National Family Health Survey Data, obtained from the Demographic and Surveys Health Program. Two datasets were used: household member recoded (individual-level) data and clusters based on latitude and longitude. There were a total of 2,869,043 respondents, 28,526 points, and 640 districts (as of the time of administration of the survey). The study population included members of households in India. The datasets were joined and overall proportions of exposures, co-variates, and outcomes were calculated per number of respondents in each district. The exposure of interest—being a member of a scheduled caste or tribe—was operationalized as dichotomous.
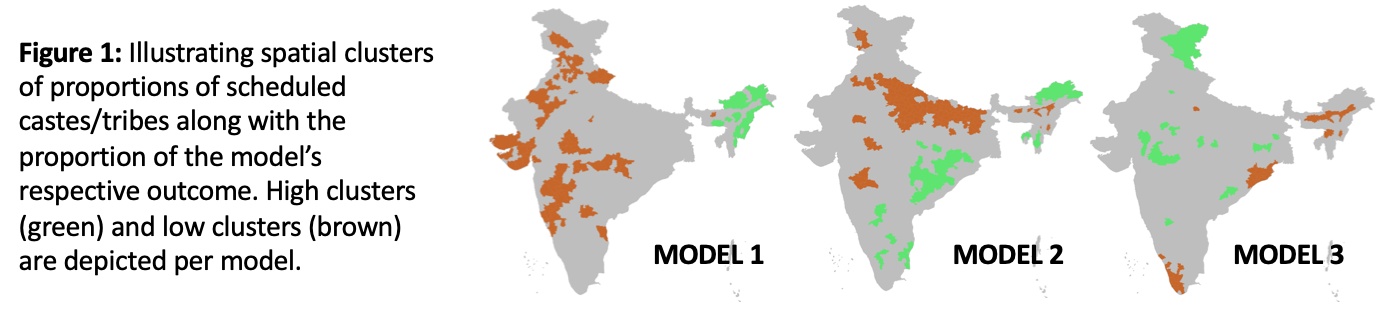
The shape file containing the districts of India was obtained from GADM, the Database of Global Administrative Areas. Initially, a local Moran’s univariate I test was ran to examine spatial neighbors using Queens’ contiguity (Moran’s I = 0.2035, p-value = 0.001).
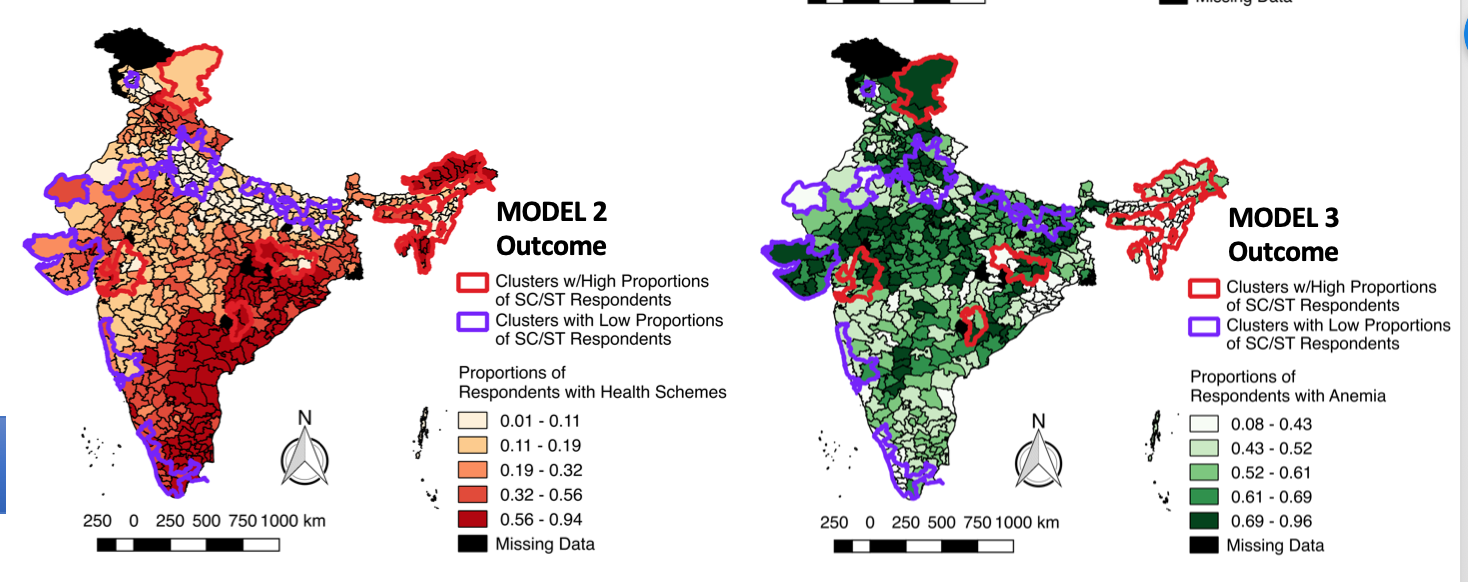
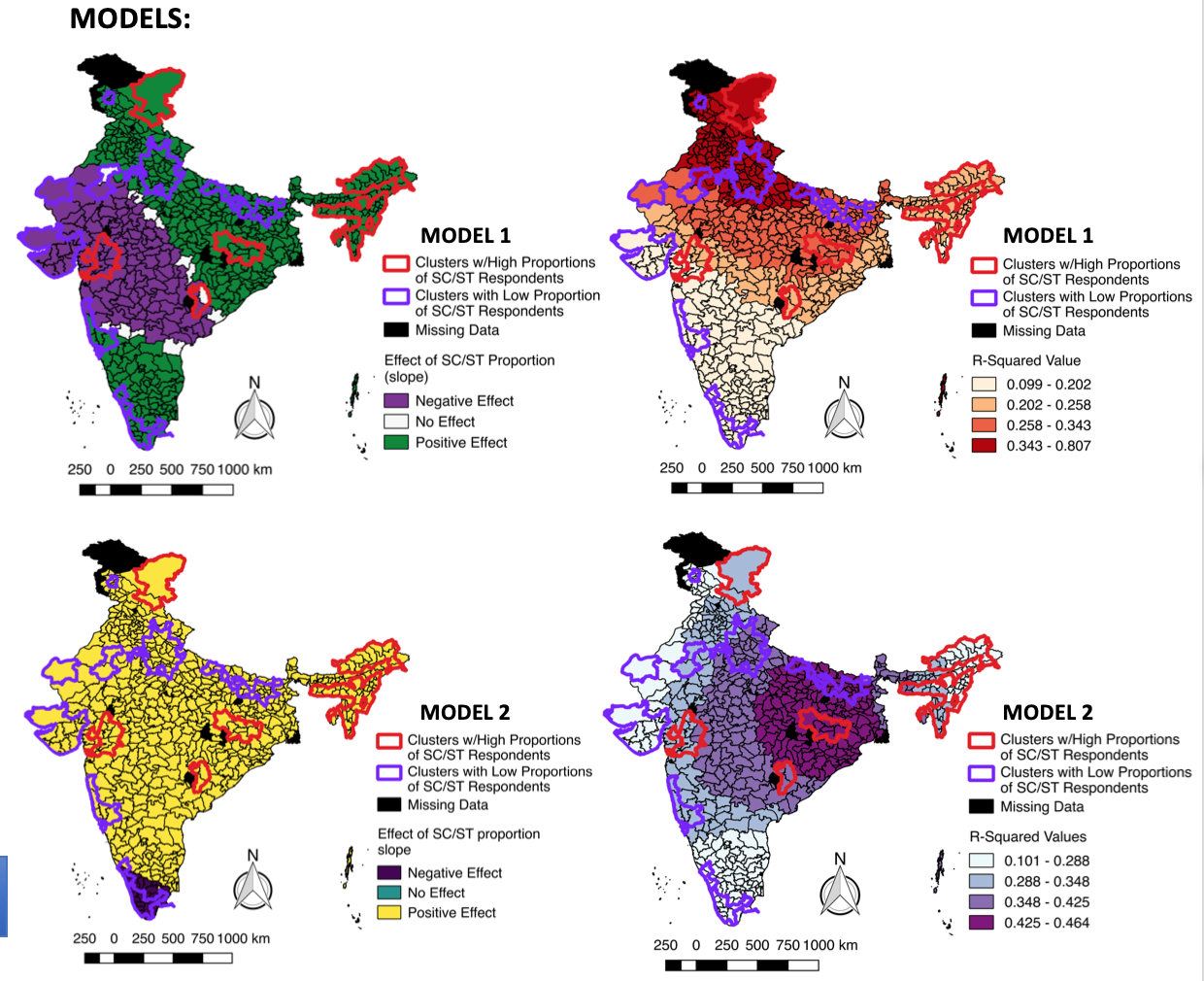
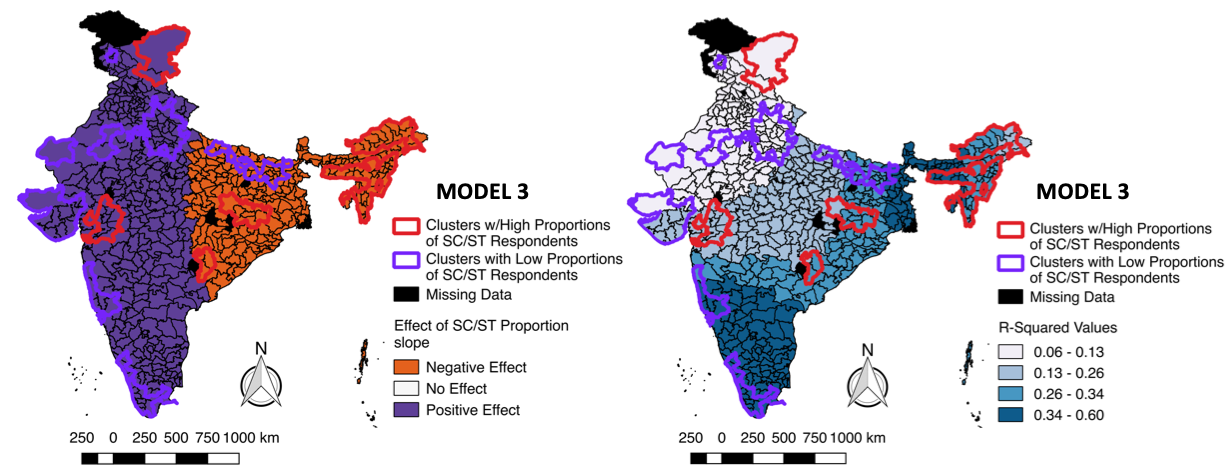
Then a local Moran’s univariate I test was ran on scheduled caste/tribe proportion to identify clusters with high and low proportions of scheduled caste/tribe populations (Moran’s I = 0.63, p-value = 0.001). Afterwards, one global regression model was run per each outcome (proportion of anemic respondents, proportion of respondents with tuberculosis, and proportion of respondents covered by a health scheme), with proportion of scheduled caste/tribe members as the main exposure, while controlling for median age of respondents per district and average wealth index of respondents per district. Then, using the R package spgwr, I ran the localized models via a geographically weighted regression approach with a Gaussian weighting scheme.
VISUALIZATIONS:
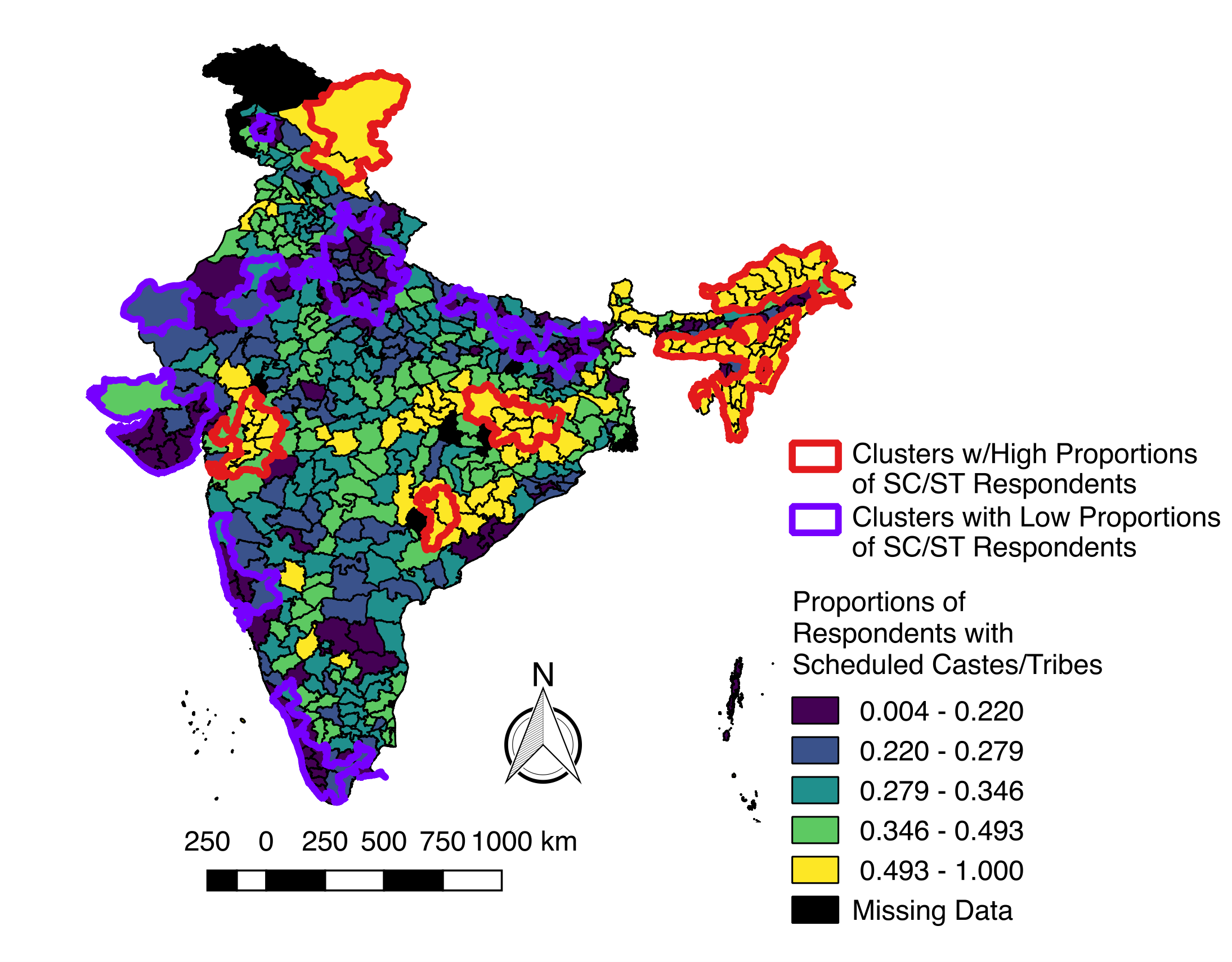
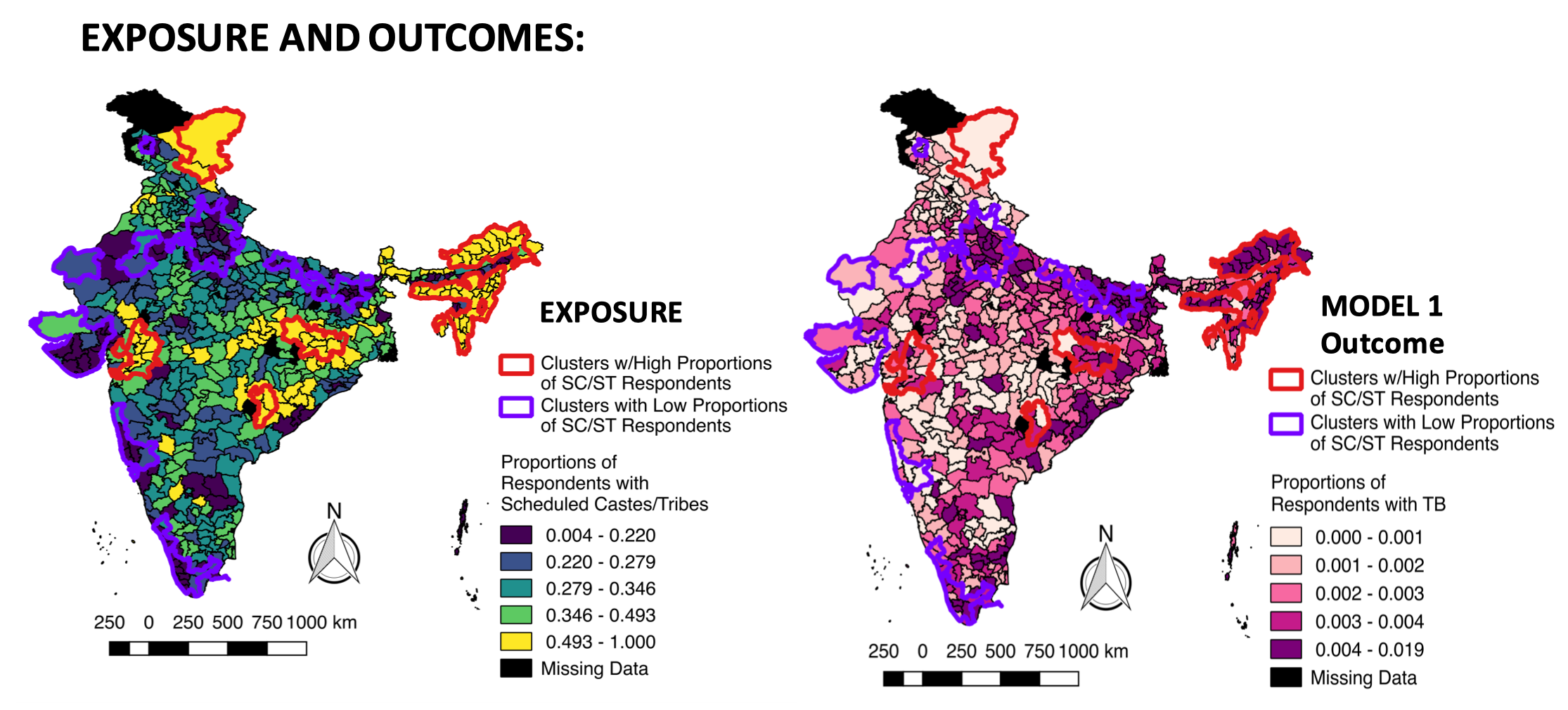
The exposure image file depicts the distribution of scheduled castes and tribes across India (based on the data from the National Family Health Survey). Statistically significant clustering is also included of areas with high and low proportions of scheduled castes and tribes. The map and data are at district levels.
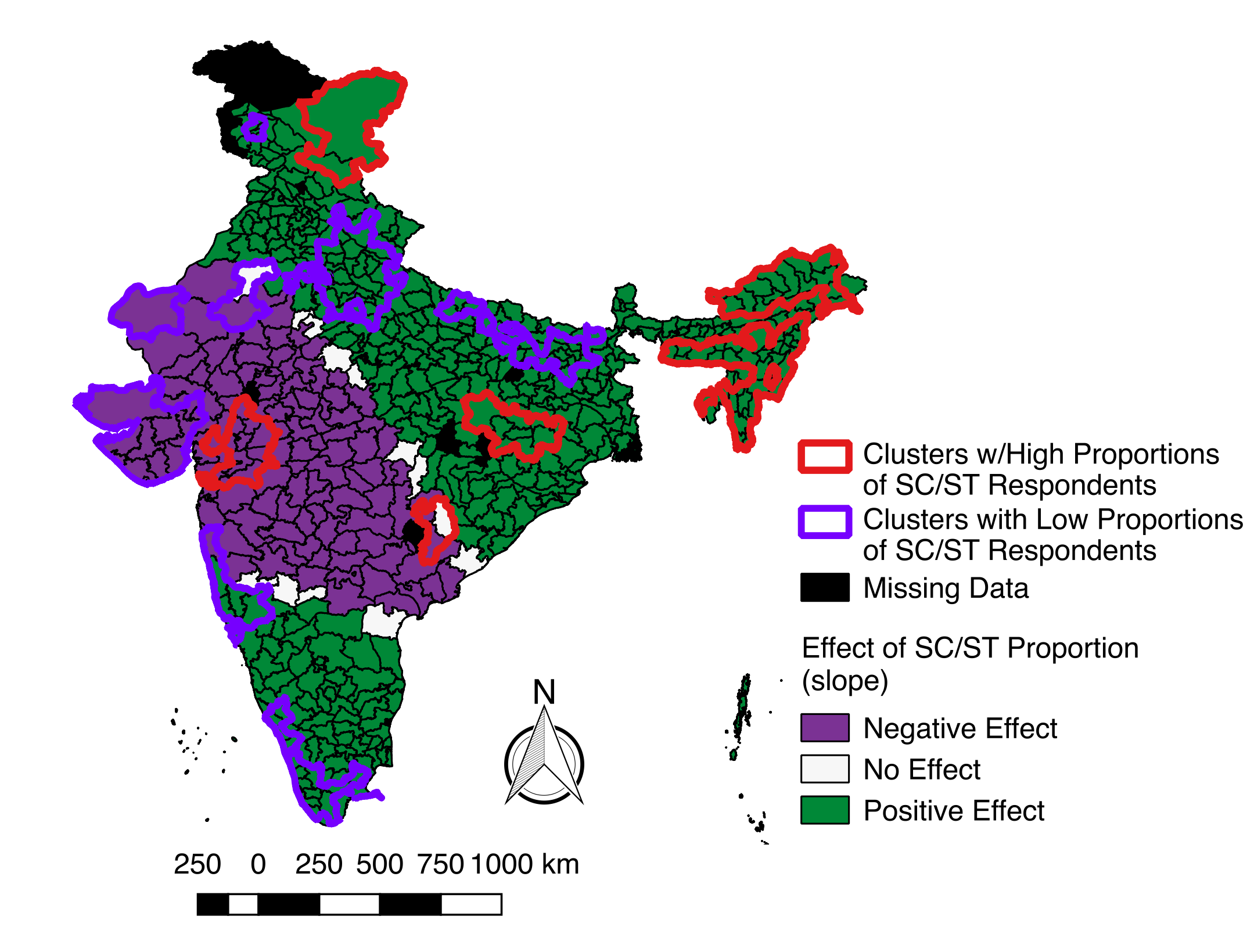
The model1 file depicts the results of a geographically weighted regression model: TB as an outcome of multiple predictors, including caste. Districts which have a positive association with proportion of scheduled castes/tribes and TB prevalence are depicted as green while districts which have a negative association with proportion of scheduled castes/tribes and TB prevalence are depicted as blue.
Descriptive Statistics
Models
Model BiVariate Analysis
Model Comparison
| Model | Outcome | R-Squared (Global Model) | Caste proportion coefficient (Global Model) | p-value caste proportion coefficient (Global Model) | Moran’s I (bivariate analysis) | p-value of (bivariate analysis) |
|---|---|---|---|---|---|---|
| 1 | Tuberculosis | 0.133709 | 0.00265737 | <0.0001* | 0.203 | 0.001* |
| 2 | Having a health scheme | 0.259311 | 0.226908 | <0.0001* | 0.134 | 0.001* |
| 3 | Anemia | 0.132751 | -0.130669 | <0.0001* | -0.211 | 0.001* |
CONCLUSION:
Discussion:
I hypothesized that based on my knowledge, the scheduled caste coefficient would have a positive effect on both TB and anemia cases, while having a negative correlation with health scheme status. Two of the three global models (health scheme and anemia) did not align with my hypothesis. However, when running local models, some districts did have coefficients in agreement with my hypothesis (which was based on my literature review). This is crucial because India’s health care policies are heterogeneous and dependent on both state and local policies. This could dictate future research in which the impact of local health policies in India on scheduled castes and tribes are evaluated.
Limitations:
Some limitations of these analyses include the loss of heterogeneity when dichotomizing castes. India contains multiple scheduled castes and tribes, all of which have experienced different forms of oppression. Disaggregating caste as a category in future health surveys could provide deeper insight into the various needs of scheduled caste/tribe communities. Additionally, this model was based on aggregate values (i.e. the median age) rather than using a clustered, multilevel analysis. Weights provided in the dataset were not used, so we also do not have assurance of external validity.
Future Research:
Future studies should disaggregate data, include population density as a variable, and consider local health policies and programs when considering the impact of caste on health.
REFERENCES:
-
GHO Key Country Indicators India - key indicators [Internet]. WHO. [cited 2019 Jan 5]. Available from http://apps.who.int/gho/data/node.cco.ki-IND?lang=en - Largest Group of Hospitals in India for Public Health care Services [Internet]. Fortis Healthcare Limited. [cited 2019 Jan 5]. Available from: https://www.fortishealthcare.com/about-us
- Mohanan M, Hay K, Mor N. Quality Of Health Care In India: Challenges, Priorities, And The Road Ahead. Health Aff (Millwood). 2016 Oct 1;35(10):1753–8.
- BARU R, ACHARYA A, ACHARYA S, KUMAR AKS, NAGARAJ K. Inequities in Access to Health Services in India: Caste, Class and Region. Econ Polit Wkly. 2010;45(38):49–58.
- Bawaskar HS, Bawaskar PH, Bawaskar PH. Health and the Indian caste system. Lancet. 2015 Jan 31;385(9966):416.
- Masoodi A. Dalit women in India die younger than upper caste counterparts: Report [Internet]. https://www.livemint.com/. 2018 [cited 2019 Jan 5]. Available from: https://www.livemint.com/Politics/Dy9bHke2B5vQcWJJWNo6QK/Dalit-women-in-India-die-younger-than-upper-caste-counterpar.html
- IIPS/India II for PS-, ICF. India National Family Health Survey NFHS-4 2015-16. 2017 [cited 2019 Jan 5]; Available from: https://dhsprogram.com/publications/publication-FR339-DHS-Final-Reports.cfm
- Race, Caste and Gender on JSTOR [Internet]. [cited 2019 Jan 5]. Available from: https://www-jstor-org.ezproxy.cul.columbia.edu/stable/2803715?seq=1#metadata_info_tab_contents
- Castes in India: Their Mechanism, Genesis, and Development, by Dr. B. R. Ambedkar [Internet]. [cited 2019 Jan 13]. Available from: http://www.columbia.edu/itc/mealac/pritchett/00ambedkar/txt_ambedkar_castes.html
- Cox OC. Race and Caste: A Distinction. Am J Sociol. 1945 Mar 1;50(5):360–8.
- Nayar KR. Social exclusion, caste & health: a review based on the social determinants framework. Indian J Med Res. 2007 Oct;126(4):355–63.
- Wheeler SM, Bryant AS. Racial and Ethnic Disparities in Health and Health Care. Obstet Gynecol Clin North Am. 2017 Mar;44(1):1–11.
- Jones CP. Levels of racism: a theoretic framework and a gardener’s tale. Am J Public Health. 2000 Aug;90(8):1212–5.
- Parker RL. Health care expenditures in a rural Indian community. Soc Sci Med. 1986;22(1):23–7.
- Kabir Z, Long J, Reddaiah VP, Kevany J, Kapoor SK. Non-specific effect of measles vaccination on overall child mortality in an area of rural India with high vaccination coverage: a population-based case-control study. Bull World Health Organ. 2003;81(4):244–50.
- Mohindra KS, Haddad S, Narayana D. Women’s health in a rural community in Kerala, India: do caste and socioeconomic position matter? J Epidemiol Community Health. 2006 Dec 1;60(12):1020–6.
- Desai S, Dubey A. Caste in 21st Century India: Competing Narratives. Econ Polit Wkly. 2012 Mar 12;46(11):40–9.
- Roy A. The Doctor and the Saint: Caste, Race, and Annihilation of Caste, the Debate Between B.R. Ambedkar and M.K. Gandhi. Haymarket Books; 2017. 145 p.
- Chalam KS, Chalam KS. Caste-based reservations and human development in India. Sage Publications; 2007. 216 p.
- Constitution of India [Internet]. [cited 2019 Jan 14]. Available from: http://www.liiofindia.org/in/legis/cen/const/2004/index.html
- The Effectiveness of Jobs Reservation: Caste, Religion and Economic Status in India - Borooah - 2007 - Development and Change - Wiley Online Library [Internet]. [cited 2019 Jan 6]. Available from: https://onlinelibrary-wiley-com.ezproxy.cul.columbia.edu/doi/full/10.1111/j.1467-7660.2007.00418.x#fn1
- In 21st century India, caste still decides what you do - Times of India [Internet]. The Times of India. [cited 2019 Jan 5]. Available from: https://timesofindia.indiatimes.com/india/in-21st-century-india-caste-still-decides-what-you-do/articleshow/67201813.cms
- Link BG, Phelan J. Social Conditions As Fundamental Causes of Disease. J Health Soc Behav. 1995;80–94.
- Bamshad M, Kivisild T, Watkins WS, Dixon ME, Ricker CE, Rao BB, et al. Genetic Evidence on the Origins of Indian Caste Populations. Genome Res. 2001 Jun 1;11(6):994–1004.
- Yadav R, Lazarus M, Ghanghoria P, Singh M, Gupta RB, Kumar S, et al. Sickle cell disease in Madhya Pradesh, Central India: A comparison of clinical profile of sickle cell homozygote vs. sickle-beta thalassaemia individuals. Hematology. 2016 Oct;21(9):558–63.
- Joshi DC, Mishra VN, Bhatnagar M, Singh RB, Garg SK, Chopra H. Socioeconomic factors and prevalence of endemic goitre. Indian J Public Health. 1993 Jun;37(2):48–53.
- Kumar S, Heath A, Heath O. Determinants of Social Mobility in India. Econ Polit Wkly. 2002;37(29):2983–7.
- Iyengar K. Early postpartum maternal morbidity among rural women of Rajasthan, India: a community-based study. J Health Popul Nutr. 2012 Jun;30(2):213–25.
- Thresia CU. Health Inequalities in South Asia at the Launch of Sustainable Development Goals: Exclusions in Health in Kerala, India Need Political Interventions. Int J Health Serv. 2018 Jan;48(1):57–80.
- Nair NS, Rao RSP, Chandrashekar S, Acharya D, Bhat HV. Socio-Demographic and Maternal Determinants of Low Birth Weight : A Multivariate Approach. Indian J Pediatr. 2000 Jan 1;67(1):9–14.
- Francis MR, Nohynek H, Larson H, Balraj V, Mohan VR, Kang G, et al. Factors associated with routine childhood vaccine uptake and reasons for non-vaccination in India: 1998-2008. Vaccine. 2018 Oct 22;36(44):6559–66.
- Shenton LM, Wagner AL, Bettampadi D, Masters NB, Carlson BF, Boulton ML. Factors Associated with Vaccination Status of Children Aged 12-48 Months in India, 2012-2013. Matern Child Health J. 2018 Mar;22(3):419–28.
- Patel P, Das M, Das U. The perceptions, health-seeking behaviours and access of Scheduled Caste women to maternal health services in Bihar, India. Reprod Health Matters. 2018 Nov;26(54):114–25.
- Kapil U, Verma D, Narula S, Nayar D, Sachdev HP, Shah AD, et al. Breast-feeding practices in Schedule Caste communities in Haryana state. Indian Pediatr. 1994 Oct;31(10):1227–32.
- Kapil U, Verma D, Sachdev HP, Nayar D, Shah AD, Gnanasekaran N. Use of milk based commercial weaning foods amongst scheduled caste communities in Haryana. Indian Pediatr. 1995 Aug;32(8):905–8.
- Arlappa N, Balakrishna N, Laxmaiah A, Brahmam GN. Prevalence of anaemia among rural pre-school children of West Bengal, India. Ann Hum Biol. 2010 Apr;37(2):231–42.
- Gosdin L, Martorell R, Bartolini RM, Mehta R, Srikantiah S, Young MF. The co-occurrence of anaemia and stunting in young children. Matern Child Nutr. 2018 Jul;14(3):e12597.
- Agarwal S, Srivastava A. Social determinants of children’s health in urban areas in India. J Health Care Poor Underserved. 2009;20(4 Suppl):68–89.
- Arlappa N, Laxmaiah A, Balakrishna N, Harikumar R, Kodavanti MR, Gal Reddy C, et al. Micronutrient deficiency disorders among the rural children of West Bengal, India. Ann Hum Biol. 2011 May;38(3):281–9.
- Kumari S. Nutritional status of scheduled caste pre-school children. Indian J Public Health. 2005 Dec;49(4):258–9.
- Mishra VK, Retherford RD, Smith KR. Biomass cooking fuels and prevalence of tuberculosis in India. Int J Infect Dis. 1999 Spring;3(3):119–29.
- Bhargava A, Benedetti A, Oxlade O, Pai M, Menzies D. Undernutrition and the incidence of tuberculosis in India: national and subnational estimates of the population-attributable fraction related to undernutrition. Natl Med J India. 2014 Jun;27(3):128–33.
- Chakrabartty A, Basu P, Ali KM, Sarkar AK, Ghosh D. Tuberculosis related stigma and its effect on the delay for sputum examination under the Revised National Tuberculosis Control Program in India. Indian J Tuberc. 2018 Apr;65(2):145–51.
- Ramakrishnan U, Lowe A, Vir S, Kumar S, Mohanraj R, Chaturvedi A, et al. Public health interventions, barriers, and opportunities for improving maternal nutrition in India. Food Nutr Bull. 2012 Jun;33(2 Suppl):S71-92.
- Saroha E, Altarac M, Sibley LM. Caste and maternal health care service use among rural Hindu women in Maitha, Uttar Pradesh, India. J Midwifery Womens Health. 2008 Oct;53(5):e41-7.
- Altijani N, Carson C, Choudhury SS, Rani A, Sarma UC, Knight M, et al. Stillbirth among women in nine states in India: rate and risk factors in study of 886,505 women from the annual health survey. BMJ Open. 2018 Nov 8;8(11):e022583.
- KRISHNAN S. Gender, Caste, and Economic Inequalities and Marital Violence in Rural South India. Health Care Women Int. 2005 Jan 1;26(1):87–99.
-
Consequences Intimate Partner Violence Violence Prevention Injury Center CDC [Internet]. 2018 [cited 2019 Jan 14]. Available from: https://www.cdc.gov/violenceprevention/intimatepartnerviolence/consequences.html - Krishnan S. Do structural inequalities contribute to marital violence? Ethnographic evidence from rural South India. Violence Women. 2005 Jun;11(6):759–75.
- Mohanty SK, Ram F. LIFE EXPECTANCY AT BIRTH AMONG SOCIAL AND ECONOMIC GROUPS IN INDIA. :2.
- Thind A, Mohani A, Banerjee K, Hagigi F. Where to deliver? Analysis of choice of delivery location from a national survey in India. BMC Public Health. 2008 Jan 24;8:29.
- Zacharias A, Vakulabharanam V. Caste Stratification and Wealth Inequality in India. World Dev. 2011 Oct 1;39(10):1820–33.
- Polit KM. The Effects of Inequality and Relative Marginality on the Well-being of Low Caste People in Central Uttaranchal. Anthr Med. 2005 Dec;12(3):225–37.
- Bhanderi MN, Kannan S. Untreated reproductive morbidities among ever married women of slums of Rajkot City, Gujarat: the role of class, distance, provider attitudes, and perceived quality of care. J Urban Health. 2010 Mar;87(2):254–63.
- Khubchandani J, Soni A, Fahey N, Raithatha N, Prabhakaran A, Byatt N, et al. Caste matters: perceived discrimination among women in rural India. Arch Womens Ment Health. 2018 Apr;21(2):163–70.
- Banda K, Sarkar R, Gopal S, Govindarajan J, Harijan BB, Jeyakumar MB, et al. Water handling, sanitation and defecation practices in rural southern India: a knowledge, attitudes and practices study. Trans R Soc Trop Med Hyg. 2007 Nov;101(11):1124–30.